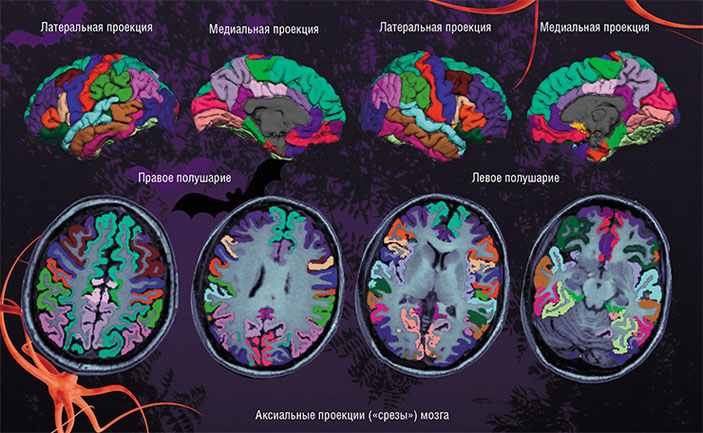
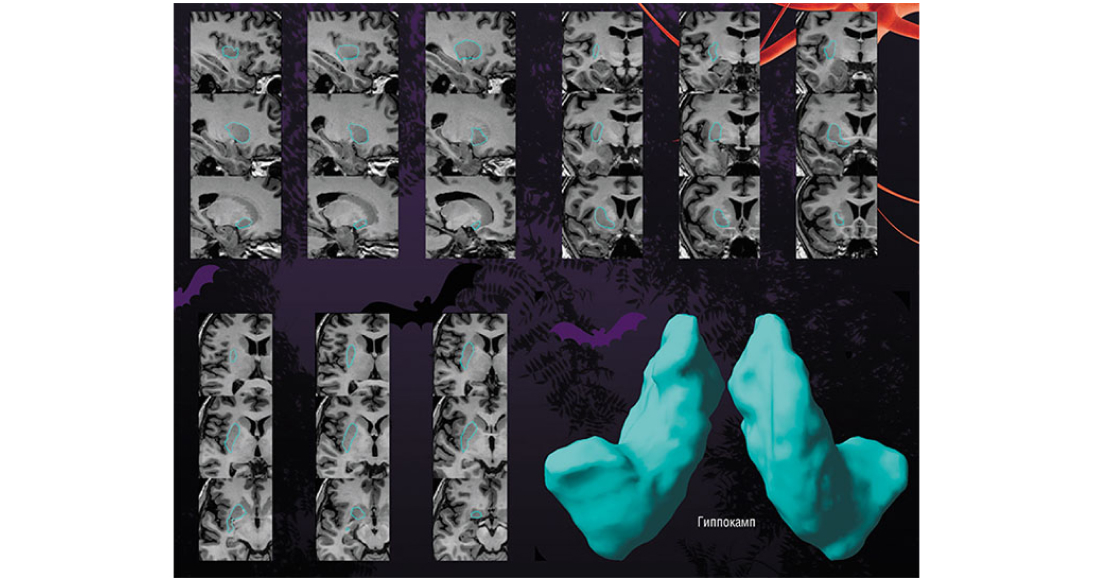
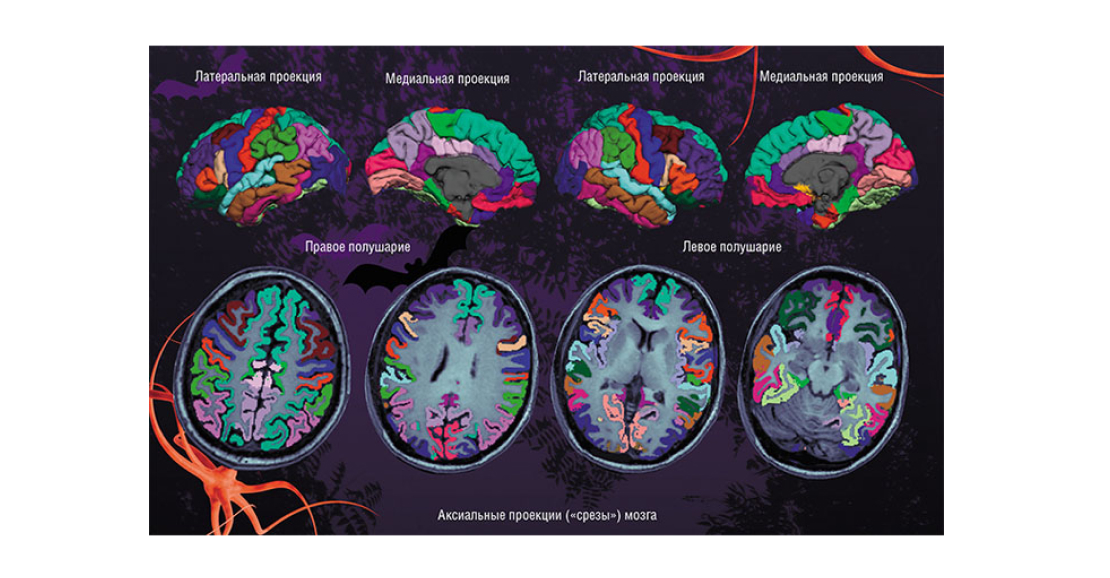
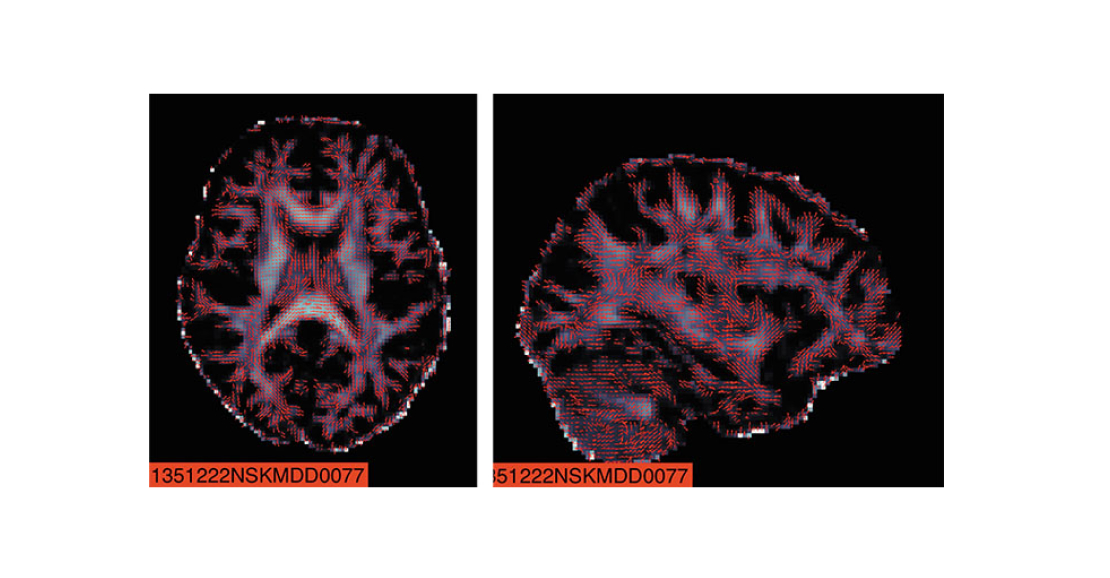
Using the Shape program to assess the individual variability of deep, subcortical brain formations in patients with depression allows us to obtain accurate quantitative estimates of their shape and size. The data was obtained as part of the ENIGMA-MDD working group
But if the medicine does not help, it must be changed urgently! Today, the effectiveness of a drug for depression is assessed mainly on the basis of clinical signs, and this can usually be done no earlier than 4-8 weeks after the start of treatment. But what if we are talking about a patient with high suicidal tendencies, which is not uncommon in the case of this disease?
According to recent data, depression is present in the structure of a wide variety of diseases: not only professional psychiatrists, but also general practitioners are often forced to deal with certain aspects of this pathology. According to reliable multicenter studies conducted using a single method in several medical institutions simultaneously, depression is one of the causes of decreased immunity and, as a result, is an important risk factor for the development of many somatic diseases, including cardiovascular and oncological. Moreover, in some cases, it plays the role of a “mask” that has been “covering up” the current pathological process for a long time.
Here, neurophysiological and neuroimaging, as well as omix markers, should come to the rescue. Omix technologies were named after the suffix “-omik”, common to advanced fields of biology such as genomics, transcriptomics, proteomics and metabolomics, which study the implementation of hereditary information at all levels of the molecular organization of a living organism, from the genome to the proteome and the metabolome (the totality of all proteins and low molecular weight metabolic products, respectively).
To determine the effectiveness of depression therapy, we can use a whole arsenal of omix markers, ranging from DNA markers of genetic polymorphism and mRNA levels to specific proteomic and metabolic characteristics. The same can be said about various clinical forms of classic neurodegenerative diseases such as Parkinson’s and Alzheimer’s diseases. In a broader sense, we are talking about the development of predictors (“predictors”) of not only the risk of occurrence, but also the nature of clinical dynamics and sensitivity to drug therapy for a number of affective and neurodegenerative diseases. Predictors and markers of high suicidal readiness should certainly be allocated to a separate group.
An example of such an approach to diagnosing the effectiveness of therapy is a study planned within the framework of the SAE “Neuroscience in Translational Medicine” at NSU. We are talking about using the characteristics of the olfactory epithelium of the patient’s upper nasal passages as a dynamic marker of the level of neuronal plasticity, which at the same time is a peripheral link of the olfactory analyzer of the brain and contains full-fledged brain neurons. Samples of such epithelium are easily obtained using a simple outpatient biopsy.
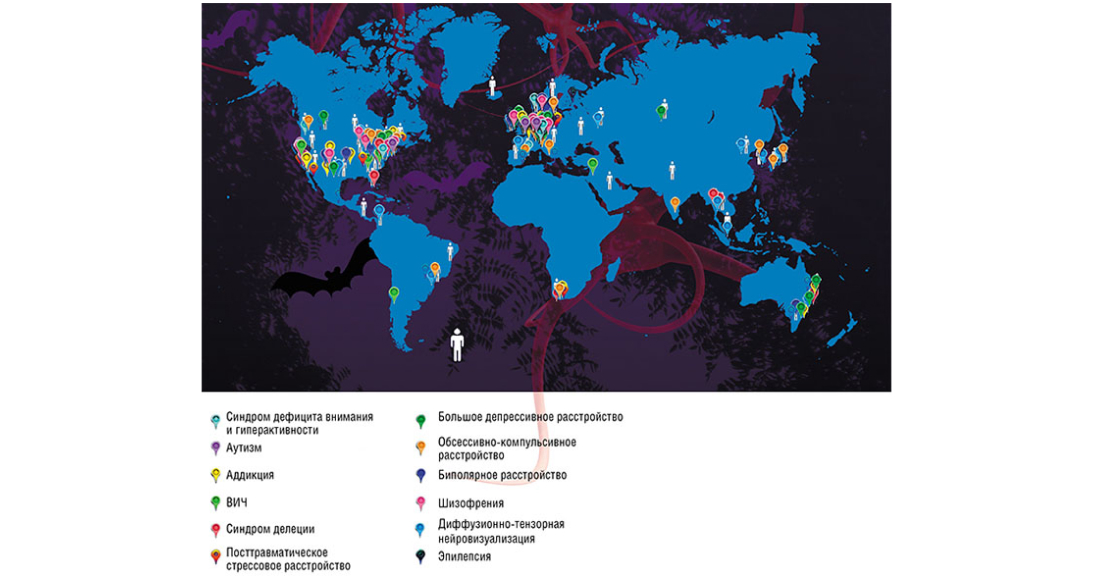
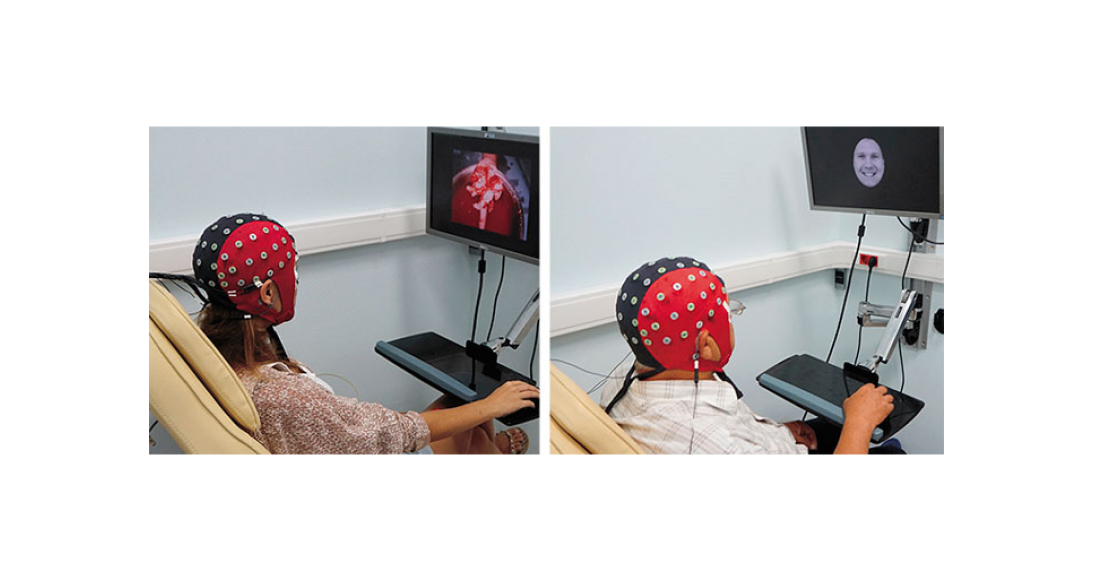
Strategic Academic Units (SAE) are scientific and educational consortia of the university, which bring together researchers who are searching in relevant scientific fields, as well as actively involved in educational activities. One of the main tasks of the SAE “Neuroscience in Translational Medicine” of Novosibirsk State University is to study the mechanisms of brain neuroplasticity, the deterioration of which is a common feature of depression and other affective and neurodegenerative diseases, the development of modern technologies for predicting the risk of these pathologies and individual sensitivity to therapy. Under the umbrella of the SAE, the NSU laboratories will work closely with research organizations from the Novosibirsk Scientific Center and the Siberian region, including academic institutes of the Siberian Branch of the Russian Academy of Sciences and Novosibirsk technoparks, with leading neurocenters in Moscow as part of large “end—to-end” projects of the NTI NeuroNet, as well as with foreign partners. Among the latter are the University of Southern California (USA), where new technologies for human—machine communication (brain-computer interface) are successfully developing, and the largest international brain research consortium ENIGMA.
Further, wide possibilities open up: we can assess the nature and dynamics of neuronal plasticity processes in response to specific drug therapy by changing the level of markers such as brain neurotrophic factor (BDNF) or mRNA. Moreover, neural progenitor stem cells can be obtained from the olfactory neuronal epithelium, cultured, and used for drug testing. As a result, in the future we will be able to assess the adequacy of prescribed medication within a few days (rather than weeks) after the start of treatment. We are already carrying out a pilot study on this topic within the framework of a grant from the Russian Science Foundation.
If a depressed patient does not respond to “pill treatment” in principle, then today there is an opportunity to resort to alternative treatment — navigational transcranial brain stimulation (rhythmic magnetic, direct or alternating current, etc.), which is a leading trend in modern clinical neuroscience. The effectiveness of these noninvasive methods in the case of drug resistance is quite high. The treatment is personalized, as all the “coordinates” of the patient’s brain scanned using MRI are transmitted to the navigation computer system. With this system, it is possible to position the coil with high (up to 1 mm) accuracy over specialized areas of the cerebral cortex involved in the development of depression and neurodegenerative diseases, and send stimulating impulses there.