Neuroprotection and neuroplasticity: new possibilities of pharmacological support
M.S. Ritsner in his book “Brain protection in schizophrenia, mood and cognitive disorders” describes the role of neuroprotection mechanisms in the treatment of diseases such as schizophrenia, mood disorders and cognitive impairments. The following review of one of the chapters of this book, written by D.F. Muresanu, presents new data on the processes of neuroprotection and neuroplasticity, as well as modern possibilities of pharmacological support for the restoration of nervous tissue.

Modern concepts of neuroprotection and neuroplasticity
Mechanisms of cell death
Currently, two main ways of cell death are described: active and passive. Necrosis is a process that can be caused by almost any pathological damage to a cell (physical, chemical, or biological in nature). The sequence of events in necrosis is always similar: osmolysis caused by cellular edema, which leads to passive death of the damaged cell. Necrosis affects not only the damaged cell, one of its secondary effects is inflammation, induced by the released cellular contents and accompanied by the production of cytokines. Another mechanism of cell death is apoptosis, which, unlike necrosis, requires the energy of adenosine triphosphate. This term comes from the ancient Greek word apoptosis and is currently used in terminology to denote a mechanism of cell death with specific morphological characteristics used by the body to control the number and quality of cells to ensure the proper functioning of organs. The nervous system is one of the best examples where the formation of the final structure and functions during development is mediated by cell death. Neurotrophic factors, in addition to influencing the vital activity of a neuron, regulate this type of cell death, thus forming the most important protective mechanism. Phenomena similar to apoptosis, in particular cellular signaling, are noted not only in neurodegenerative diseases, but also in some acute processes (trauma or stroke), also accompanied by degeneration and death of neurons. There are clear differences between apoptosis and necrosis, the most significant of which is the temporal aspect — the processes of apoptosis take place over a longer period of time than necrosis. Sometimes, when cells die, there are features inherent in both necrosis and apoptosis processes. For the same damaged neurons, the phenomena of rupture of cell membranes and fragmentation of their DNA are described, demonstrating the processes of necrosis and apoptosis, respectively. Today, the inadequacy of the generally accepted terminology of cell death processes is obvious. To denote cell death, characterized by the activation of intracellular mechanisms without changing cell morphology, Slo.iter proposed the term “active cell death”, and the author suggests replacing the outdated concept of “necrosis” with the term “passive cell death”. The relationship between pathophysiological mechanisms and types of cell death can be summarized as follows: excitotoxicity, as well as inflammation, can cause necrosis and apoptosis-like cell death, while protein folding disorder induces only apoptosis-like death.The main biological endogenous processes and endogenous protective activity
The most significant neurobiological processes that simultaneously occur under genetic control are neurotrophy, neuroprotection, neuroplasticity, and neurogenesis. They form an endogenous protective activity (EZA) designed to resist pathophysiological processes.- Neurotrophy is a natural process that implies the constancy of correct DNA expression and the preservation of a normal cell phenotype.
- Neuroprotection is a complex of mechanisms that counteract damaging factors.
- Neuroplasticity is the constant adaptation of a cell to new functional conditions. Some authors, in particular Kali.as .olkow, Muresanu, suggest the brain’s ability to change existing structures in response to an external stimulus (including learning, acquired experience, or damage).
- Neurogenesis is the formation of new cells of the nervous tissue (neurons, astrocytes and oligodendrocytes) from stem cells. The ultimate purpose of neurogenesis is the formation of new neurons.
Neuroprotection
All pathophysiological mechanisms are triggered by various etiological factors or biological events, which contributes to the occurrence of many neurological diseases with different course (acute or chronic). The purpose of neuroprotective treatment is to block these pathogenetic processes. There are several pathophysiological mechanisms that lead to the development of many diseases of the central nervous system (Table 1). These include: excitotoxicity, the appearance of free radicals, metabolic disorders, folding of protein molecules, inflammation, apoptosis-like processes. Thus, in stroke, excitotoxicity, oxidative stress, inflammation, and apoptosis-like cell death are observed. Neurodegenerative diseases are accompanied by excitotoxicity, inflammation, apoptosis-like death, and protein folding disorders. In neuropathology, the presence of excitotoxicity, inflammation, and apoptosis-like death of spinal cells has also been noted. The relief of these processes is the key to successful neuroprotective therapy of any neurological disease. The classical strategy of neuroprotective treatment is the suppression of pathophysiological mechanisms. For this purpose, drugs are used that effectively stop one of these pathophysiological processes. The rationality of this strategy is based on the harmfulness of any pathophysiological process. However, the clinical results of neuroprotective therapy are very disappointing, since the main pathophysiological mechanisms are characterized by duality. Hawkins and Da.is A relatively new concept in the field of neurophysiology called the “neurovascular unit” has been proposed. It consists of endothelial cells, brain cells, and extracellular matrix, and functions as a single unit through biochemical signaling. Such units are ubiquitously represented in the brain in gray and white matter. Disruption of their functions can explain the occurrence and development of certain brain diseases, including stroke, vascular dementia, migraine, traumatic injuries, all neurodegenerative disorders, and even natural aging processes. Since the neurovascular unit is unique, the death of the cells that make up it is also unique. Frisch and Screaton believe that the lack of support for any component of this unit (both cells and extracellular matrix) leads to the launch of such a form of apoptosis-like process as anoicosis.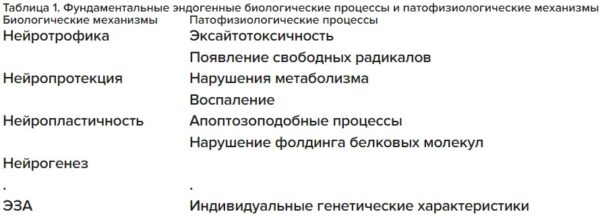
Excitotoxicity
Excitotoxicity is a pathological process in which cells of the nervous tissue are damaged due to their excessive stimulation by glutamate and similar substances. Activation of NMDA receptors is one of the distinguishing features of excitotoxicity. Wu et al. It is believed that prolonged activation of NMDA receptors is key to maintaining cell life and is achieved through the regulation of neurotrophic and neuroplasticity mechanisms through calcium-mediated systems of proteolytic enzymes (in particular, calpain). Normally, the synaptic activity of NMDA receptors is responsible for the minimal entry of Ca2+ ions into the cell, thereby contributing to the survival of neurons. Trace concentrations of calcium activate molecules with high affinity for calcium ions, such as microcalpine, thus triggering proteolytic activity. Proteolytic activity is an important link in the processes of neurotrophy and neuroplasticity and, according to Hutter et al., is specifically regulated by neurotrophic factors. Hetman and Khareba.a suggest that the key mechanisms for maintaining cell life with the participation of NMDA receptors are necessary for the realization of neurotrophy and neuroplasticity. Brunet et al. NMDA receptor activation of the phosphatidylinositol 3 kinase (PI3K) cascade, the Akt protein kinase, is considered acceptable for many, although not all types of neurons. Hardingham et al. It is confirmed that synaptic signaling through NMDA receptors activates the kinase cascade regulated by extracellular signal 1/2 (RasERK1/2), which ensures cell survival by subsequent activation of the transcription factor CREB, inactivation of the pro-apoptotic factor BAD, and inhibition of GSK3b (kinase 3bglycogen synthase) —mediated apoptosis. Hardingham et al. It has been shown that the intracellular concentration of Ca2+ ions mediated by NMDA receptors triggers multiple transcription changes, providing long-term neuroprotection (through gene expression by a CAMP-dependent mechanism). Pathological glutamate hyperactivation of NMDA receptors (for example, in stroke or traumatic injury) increases the intracellular concentration of Ca2+ ions and the activation of molecules with low affinity for calcium ions, in particular microcalpine. Such uncontrolled and non-selective proteolytic activity leads to cell death. There are several basic mechanisms of cell death mediated by NMDA receptors. An apoptosis-like process causes mitochondrial dysfunction, manifested by hyperactivation of the mitochondrial calcium uniporter and excessive uptake of Ca2+ from the cytosol. Finally, hyperactivation of calcium—dependent neuronal NO synthetases mediated by NMD receptors triggers toxic processes such as the cascade of MARkinase p38 (mitogen-activated protein kinase p38), mitochondrial dysfunction, activation of the protein family of TRP channels, melastatin, and ultimately causes apoptosis-like cell death. Next, we will consider in which cases these mechanisms ensure cell survival (neurotrophy and neuroplasticity), and in which cases they induce cell death (excitotoxicity). The first factor is the degree of NMDA receptor activation (its intensity or duration). A low level of activation is associated with the triggering of neuroprotection mechanisms. Activation of the systems responsible for cell survival requires significantly lower concentrations of Ca2+ ions than for systems leading to cell death. So, to activate the PI3K, ERK1/2 and CaMKI cascades. (calcium/calmodulin—dependent kinase type I.) — CREB – the intracellular concentration of Ca2+ ions should be significantly lower than the concentration leading to toxic processes such as activation of calpain, mitochondrial dysfunction, or synthesis of NO. Soriano et al. Information about the low calcium affinity of some strong inducers of cell death, in particular, microcalpine and the calcium uniporter of mitochondria, is confirmed. The second important factor is the location of NMDA receptors. Extra-synaptic activation of NMDA receptors dephosphorylates and inactivates the CREB transcription factor, which promotes early toxicity (in particular, mitochondrial depolarization) and, in combination with inactivation of the ERK1/2 cascade, causes necrosis or apoptosis-like cell death. On the other hand, synaptic activation of NMDA receptors activates the CREB transcription factor and the ERK1 cascade./2. Such activation does not affect the functioning of mitochondria, but it has a neuroprotective effect, and also enhances the processes of neurotrophy and neuroplasticity.Inflammation
For most neurological disorders, the pathological role of inflammation is generally recognized. A carefully controlled process that occupies a borderline state between physiological and pathological mechanisms can become quite destructive in cases of prolonged course or insufficient regulation. At the same time, inflammatory cells, as well as inflammatory mediators, play an important role in tissue repair processes. The main mediators of the positive effect of inflammation on the processes of neuroprotection and neuroplasticity are neurotrophic factors. Masson et al. The involvement of neurotrophic factors secreted by activated cells of the immune system in the processes of neuroprotection and neuroplasticity has been demonstrated. These factors can act both directly by binding to specific receptors and by modulating the local immune response. Arnett et al. and Marchetti et al. It is believed that even molecules with pronounced pro-inflammatory effects, such as tumor necrosis factor a (TNFa), have neuroprotective and neurotrophic effects (in the case of activation of R2 receptor subunits). The blood-brain barrier has a very low permeability to immunocompetent cells and molecules. Usually, in the central nervous system, immune reactivity is regulated by microglial cells and astrocytes. Other substances can enter the central nervous system only as a result of highly regulated processes mediated by adhesion molecules, chemokines, cytokines, and matrix metalloproteases.Apoptosis and apoptosis-like processes
Apoptosis is a natural physiological process aimed at maintaining a certain number and quality of cells. When DNA is damaged in a cell, the p53 gene is activated. Such a cell either stops in the G1 phase of the cell cycle (when the anti-apoptotic protein bcl2 is activated) until the damaged DNA is repaired and then repeats its cell cycle, or when DNA repair is impossible, the pro-apoptotic protein bax is activated, followed by the induction of apoptosis. If apoptosis does not occur, such a cell begins to divide uncontrollably, eventually forming a malignant neoplasm. Based on the above statements about the existence of a relationship between pathophysiological processes and EZA, the following conclusions can be drawn:: Activation of NMDA receptors has a positive effect on the processes of neuroprotection and neuroplasticity (with physiologically normal activation) and a negative effect (with hyperactivation) by increasing excitotoxicity, which leads to the development of pathological processes such as stroke, traumatic injuries, and neurodegenerative diseases. Inflammation in general has a negative effect, but it can also positively affect the processes of neuroprotection and neuroplasticity through the release of neurotrophic factors. Apoptosis is a natural physiological process, while apoptosis—like death is always pathological. Apoptosis-like processes are controlled both by endogenous mechanisms and by medication. Thus, the best strategy for therapeutic neuroprotection is the use of pleiotropic drugs that modulate (but not suppress) pathological disorders. Such drugs should suppress excitotoxicity that develops upon stimulation of non-synaptic NMDA receptors, reduce the negative and potentiate the positive effects of inflammation, and prevent the development of apoptosis-like processes. Drug development is difficult for a number of reasons. First, synthetic molecules are used that are not used in EZA, which have only one mechanism of action on complex cascading processes. Since such molecules inhibit both negative and positive biological mechanisms of pathophysiological processes, it seems unlikely to create drugs based on them with a broad neuroprotective effect. Secondly, the methodology of clinical trials of neuroprotective agents should be tightened. Grotta believes that despite the lack of consistent data on the effectiveness of neuroprotective drugs based on such synthetic molecules, some clinical studies have shown their effectiveness (in particular erythropoietin, cerebrolysin and citicholine). All of the above molecules have proven effectiveness and have a similar effect: due to the pleiotropic mechanisms of action, they are able to control many pathophysiological processes of biological cascade mechanisms. Of all such molecules, only neurotrophic factors are able to modulate (but not suppress) pathophysiological processes, potentiating their positive effects. Another advantage of neurotrophic factors is their uniqueness in stimulating neuroprotection processes and the possible switch to stimulating neuroplasticity. Such a switch to stimulation of plastic processes is an extremely important therapeutic effect in the treatment of patients. Drugs with this property are called “multimodal”, they are able to simultaneously regulate two or more basic biological processes of EZA. The multimodal drug cerebrolysin used in clinical practice contains active fragments of various neurotrophic factors. It is known that in stroke, glutamate has a detrimental effect from the first minutes to several hours after the attack. After 4872 hours, glutamate becomes the main inducer of nerve tissue repair processes. Thus, multimodal tools should be able to switch from the control of neuroprotection processes to the control of neuroplasticity within a single EZA process.Neuroplasticity and restoration of nervous tissue in neurological diseases
The EZA of the nervous system is a multiple long—term process consisting of simultaneous neurobiological processes such as neurotrophy, neuroprotection, neuroplasticity and neurogenesis. The result of the combined action of these processes is considered to be the regeneration of nervous tissue. The restoration of nervous tissue is a positive clinical outcome and is characterized by rapid functional and delayed structural effects. The realization of rapid and delayed effects leads to two types of changes: restoration and substitution. Restoration is an internal process involving biochemical and genetic mechanisms and is manifested by a decrease in swelling, absorption of gemma, restoration of axonal transport and ion current. According to Barnes et al., the substitution process is associated with the presence of an external stimulus such as training, under the influence of which the mechanisms of acquired plasticity are realized through training. Compensation is a process designed to adjust the damaged skills of the patient to his needs and the needs of the environment.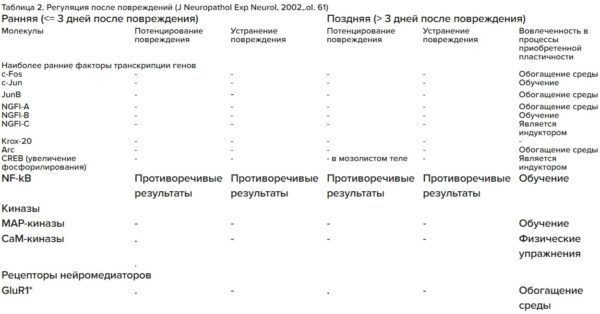
Don’t miss the most important science and health updates!
Subscribe to our newsletter and get the most important news straight to your inbox
Published
June, 2024
Duration of reading
About 5-6 minutes
Category
The brain and nervous system
Share
Biological aspects of nerve tissue repair
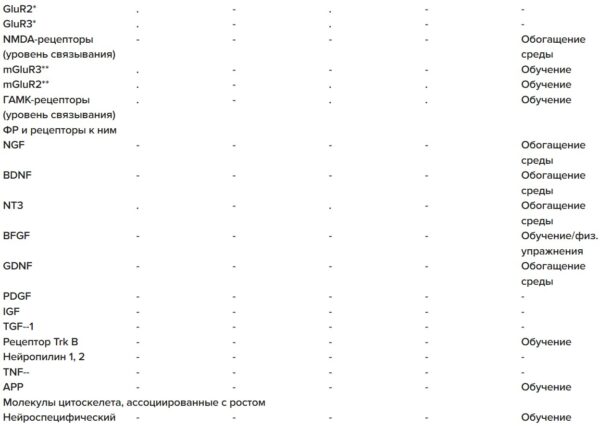
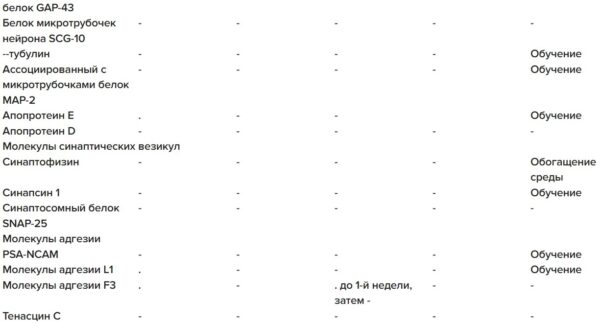
All basic biological mechanisms can be physiologically activated by endogenous or exogenous stimuli. Dysregulation of any of the four main mechanisms of EZA leads to the development of pathological processes. According to Read et al., disruption of both positive and negative regulation of neuroplasticity processes contributes to the development of pathologies. The physiological regulation of these processes is carried out by such endogenous effectors as neurotrophic factors and neurotrophic-like molecules. In order to improve the well-being of patients, effectively suppress pathological processes and support the processes of restoring nervous tissue, EZA must be exogenously stimulated with pharmacological drugs, physiotherapy, electromagnetic stimulation, psychological support, stimulation by environmental factors, stem cell transplantation or a combination of the above stimuli. In order to achieve the greatest effectiveness of stimulating two successive EZA processes — neuroprotection and neuroplasticity — it is necessary to develop pleiotropic and multimodal pharmacological preparations containing molecules with similar structures and functions to endogenous molecules. In the brain, the processes of neuroprotection and neuroplasticity occur with the involvement of the same neurotrophic factors, but in different combinations. Activation of such factors occurs due to changes in gene expression against the background of damage. According to Danton, Dietrich, and Ginsberg, brain ischemia shows the greatest change in gene expression among all pathologies. However, after damage, the protein products of many activated genes are not translated. The maximum effectiveness of endogenous neuroprotection is maintained for 72 hours after a stroke. All subsequent positive clinical outcomes are mediated by neuroplasticity and neurogenesis. A brief overview of post-injury regulation is given in Table 2. It is often difficult to identify the time of the onset of individual changes (early or late), to interpret their impact. Early changes seem to characterize the activation of neuroprotective mechanisms in response to cell damage and have little effect on the magnitude of the recovery potential. The late changes are indicative of the recovery process as a whole, but the overlap of different processes and their complexity make it difficult to identify individual changes. Regarding gene expression, it should be noted that expression changes occur at the level of entire clusters, rather than individual genes. Ginsberg emphasizes the importance of the fact that one of the distinguishing features of endogenous programs is their flexibility. In a simplified form, 72 hours is considered as a key time interval: the first 72 hours after a stroke represent a time window of early changes, and all events occurring after that are classified as late.Pharmacological support of nerve tissue repair processes
Neurotrophic factors play an important role in the recovery process. More than one hundred neurotrophic-like molecules are grouped into various families. Neurotrophic factors act by binding to specific receptors; as a rule, they are able to interact with two or more. Some of them have a high affinity for neurotrophic factors, while others are low affinity. Binding to each of them triggers an intracellular cascade of biochemical reactions, eventually leading to the activation of transcription factors. Transcription factors are DNA-associated proteins that control gene expression. According to Millan and Arenillas, when cells are stimulated, biochemical modifications of the structure of these molecules occur, as a result of which they acquire the ability to penetrate the cell nucleus, bind to various cofactors, etc. Apart from neurotrophic factors, none of the synthetic or biological drugs are able to stimulate the processes of neuroprotection and neuroplasticity.Conclusions
- The final post-traumatic changes are highly individual. Xerri et al. It is believed that the degree of cortical reorganization and recovery depends on the presence of previous damage and the possible influence of genetic factors.
- Recent studies using functional magnetic resonance imaging and positron emission tomography have shown that functional compensation occurs in the presence of extensive reorganization of the activity of the damaged brain.
- The effect of “sequential damage” is widespread in animals and humans, in which damage occurs progressively at various stages. For example, a month after extirpation of the frontal cortex of the left hemisphere, homologous sections of the cortex of the right hemisphere are destroyed. In this case, animals and humans have better and greater preservation of functions than with similar injuries occurring simultaneously.
- In most cases, clinical visualization of even extensive, slowly growing lesions is significantly difficult, and sometimes impossible). In acute injuries such as stroke or traumatic brain injury, such problems do not arise. Based on the differences in functional and clinical outcomes of acute and chronic injuries, Kolb et al., Beaulieu concluded that functional reorganization is independent of a certain type of cerebral cortex and the equipotential of the regenerative function of the central nervous system.
- Kolb et al. They emphasize the need for rehabilitation therapy at the appropriate time for each individual injury.

